The Institute for Health Policy and Practice's efforts in the area of Health Analytics and Informatics transforms health data into actionable information to support data-driven decision-making.
For more information, contact Deborah Fournier at deborah.fournier@unh.edu
Projects and Initiatives
To better understand a broad range of issues related to the cost and utilization of health care services, IHPP maintained a suite of analytic reports based on NH medical, pharmacy and dental claims data. The NH Claims Report Suite contained measures of types of service, burden of specific diseases and conditions, and use of medications, with the ability to drill down by population and geographic characteristics. This work was funded with support from the Endowment for Health and the New Hampshire Department of Health and Human Services (NH DHHS). To learn about the project, please contact Erica Plante. To learn more about the commercial claims data, visit nhchis.com.
Suggested citation: Institute for Health Policy and Practice. (2020). NH Claims Report Suite. [Dashboard]. Durham, NH: Center for Health Analytics and Informatics.

Analytics for NH Department of Health and Human Services
Our team provides analysis of claims data to DPHS in an effort to study prevalence, cost and utilization of healthcare services for several chronic diseases, including diabetes, hypertension and cancer from Medicare, Medicaid and commercial claims data.
- Cost and Utilization of Treatment for Diabetes in New Hampshire: Analysis of Medical and Pharmacy All-Payer Claims Data
- Health Care Claims and Mental Health ED Utilization
We are also providing claims data analysis for a study of behavioral-health related mortality in Medicaid, a joint project between the Division of Public Health Services and the Office of Medicaid.
Quality Assurance for NH All-Payer Claims Data (APCD)
IHPP develops protocols and completes the QA process for NH CHIS data to support the work of the NH Department of Health and Human Services.
NH Medicaid Quality Information System
With funding from the Centers for Medicaid and Medicare Services Adult Medicaid Quality program, IHPP is contracted with NH DHHS to develop and maintain the NH Medicaid Quality Information System.
HealthWRQS

IHPP partnered with the NH Department of Health and Human Services to support NH HealthWRQS, a web-based query analysis system that allows public health practitioners the ability to query data and view reports instantly about the health of New Hampshire communities.
Resources and Publications

Covering the Care: Pregnancy Tops the List of Highest Out-Of-Pocket Costs for NH’s Commercially Insured
February 2025
This data brief presents a retrospective analysis of available medical claims data from New Hampshire’s commercial insurance plans. This brief focuses on conditions with the highest average out-of-pocket costs paid by commercially insured members in 2022. It also examines how out-of-pocket costs for those conditions have changed over a seven-year period (2016-2022). The analysis is based on claims data from January 2016 – December 2022 and is analyzed at the overall population level and by member gender. It is part of a series of analytic briefs examining the rate of the most common health conditions and treatment costs for those respective conditions.

Covering the Care: Pharmaceutical Utilization and Per-Member-Per-Month Costs
January 2025
This data brief presents a retrospective descriptive analysis of pharmaceutical utilization and its associated costs by utilizing available pharmacy claims data from three of New Hampshire’s insurance payers: commercial, NH Medicaid, and NH Medicare. The brief identifies the top ten drug classes by number of prescriptions filled and their per-member-per-month costs. The analysis is based on the most recent calendar year of pharmacy claims data available (January – December 2022).
Covering the Care: Pharmaceutical Utilization and Per-Member-Per-Month Costs

Covering the Care: Most Costly Health Conditions – Metabolic Disorders, Hemophilia, Cancers, and Transplants Top the List
February 2025
This data brief presents a retrospective analysis of available medical claims data from New Hampshire’s commercial, Medicaid, and Medicare insurance programs. This brief focuses on the conditions that incur the highest medical costs, regardless of their prevalence among the population. Metabolic disorders, hemophilia, certain cancers, and transplants were identified across all three payers as some of the costliest conditions. Most of these conditions have low prevalence and could, in some instances, be considered rare. There is variability in the prevalence of these conditions by payer type and there is a variability in the costs paid by payer type, with commercial insurance consistently having the highest costs. The analysis uses administrative medical claims data from January to December 2022.
Assessment Tools for Evaluating Primary Care Services and Delivery from the Consumer and Provider Perspective
February 2024
Develop a synthesis of tools and recommendations for collecting data from patients and clinicians related to primary care services and care delivery. Create a report of recommended tools that have been used and validated, ideally with an appendix of the actual survey instruments when they are available and can be used either with permission or for a fee.
February 2024
As a part of the Endowment for Health’s comprehensive strategy to improve the health of the people in New Hampshire (NH), the foundation invests in the University of New Hampshire Institute for Health Policy and Practice Health (UNH IHPP) to research and inform statewide health law and policy. Specifically, funding in 2023 focused on the provision of primary care in NH, which IHPP addressed through two reports and a focus group. The reports included a landscape on existing best-practice literature in primary care and, a review of assessment tools for evaluating primary care services and delivery. This paper provides a summary and findings of the focus group.
September 2023
A shortage of specialty providers and numerous barriers to care access have resulted in a lack of essential youth behavioral health care in New Hampshire. Over the past decade, there have been efforts across NH to address this through Behavioral Health Integration (BHI), from multi-year initiatives to practice-level training or self-funded quality improvement projects. Despite the best efforts of many, the resulting increase in service capacity has been extremely limited. In order to inform future work in BHI, this assessment compiles the experiences, thoughts, and beliefs of primary care professionals and payers pertaining to the current availability, delivery, and payment methodologies of behavioral health services in primary care.
The Current State of Behavioral Health in Primary Care for NH Youth Report
September 2023
Investing in Primary Care: Advancing Nursing Education Workforce
September 2023
NH Children and Teens Experiencing Mental Health Disorders: An Analysis of 2019-2021 Health Care Claims Data
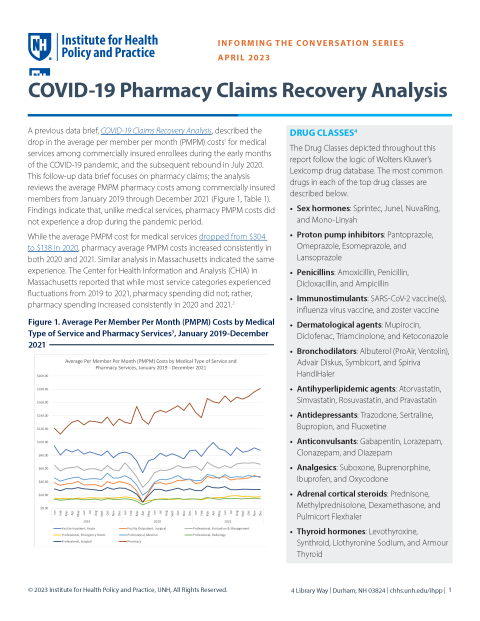
April 2023
COVID-19 Pharmacy Claims Recovery Analysis
January 2023
COVID-19 Claims Recovery Analysis
December 2022
In April of 2022, the Institute for Health Policy and Practice (IHPP), in collaboration with the Department of Health and Human Services (DHHS) and the NH Pediatric Improvement Partnership (NH PIP), published the first version of the Mental Health Care Access in Pediatrics (MCAP) report, New Hampshire Children and Teens Experiencing Mental Health Disorders: An Analysis of 2019 Healthcare Claims Data. This report builds on the work of that publication, providing an analysis that explores care patterns in 2020, at the beginning of the 2020 COVID-19 pandemic. This update also includes an additional section focused on the providers of mental health care based on medical and pharmaceutical claims data.
New Hampshire Child and Teen Mental Health: An Analysis and Comparison of 2019-2020 Healthcare Claims Data

April 2022
The NH Mental Health Care Access in Pediatrics (MCAP) program is a collaborative effort of the NH Department of Health and Human Services and the NH Pediatric Improvement Partnership housed at the UNH Institute for Health Policy and Practice. Funded by the Health Resources and Services Administration, the focus of MCAP is to promote behavioral health integration in pediatric primary care. MCAP provides: 1) training to pediatric and family practice clinicians in assessing and treating common pediatric mental health conditions through an annual Project ECHO® learning series, 2) clinician-to-clinician teleconsultation services, and 3) an annually updated referral directory of pediatric mental/behavioral health services in New Hampshire. To inform its programming, MCAP funded this analysis of 2019 pediatric medical and pharmacy claims data from commercial and NH Medicaid payers. Specifically, MCAP sought to examine health care claims for NH’s pediatric population to provide a descriptive analysis of:
- The burden of pediatric mental health conditions as defined by the percentage of children under age 18 with mental health conditions,
- Mental health conditions and comorbidities with other mental health conditions, and
- Mental health medical and pharmaceutical service utilization to produce measures of treatment.
August 2021
The Center for Health Analytics, with funding from the Children's Health Foundation, has published their oral health report which analyzes dental claims to understand patterns of oral health care services, in addition to use of fluoride and patterns of care during the COVID-19 pandemic.
March 2021
The Center for Health Analytics (CHA) at the Institute for Health Policy and Practice (IHPP) has released a new report, Cost and Utilization of Treatment for Diabetes in New Hampshire: Analysis of Medical and Pharmacy All-Payer Claims Data. By utilizing tables from IHPP's NH Claims Report Suite, CHA analyzed measures of cost and utilization for Commercial (NHCHIS), NH Medicaid and NH Medicare beneficiaries who are indicated to have diabetes and/or the related heart conditions of Congestive Heart Failure, Hypertension and Cardiovascular Disease. This report includes an overview of how diabetes and the selected heart conditions compare to the 20 most common conditions for each payer population as well as a comparison of costs and utilization of drugs classified as anti-diabetic agents to the top 10 drug classes by total scripts. The report also analyzes variations of costs for beneficiaries with diabetes or the selected heart conditions with and without co-morbidities. This project was funded by the Division of Public Health Services at NH Department of Health and Human Services.
June 2020
The Institute for Health Policy and Practice, leveraging the UNH Survey Center's Granite State Panel, conducted a survey of NH adults to understand some of the immediate impacts of COVID-19 since January 2020. The survey includes 1155 respondents, and was fielded from April 16-20, 2020.

2020
To better understand a broad range of issues related to the cost and utilization of health care services, IHPP maintains a suite of analytic reports based on NH medical, pharmacy and dental claims data. The NH Claims Report Suite contains measures of types of service, burden of specific diseases and conditions, and use of medications, with the ability to drill down by population and geographic characteristics. This work was funded with support from the Endowment for Health and the New Hampshire Children's Health Foundation. For more information about the data sources, please see the methods tabs within the report suite. To learn more about the commercial claims data, visit nhchis.org.
2017
A shortage of specialty providers and numerous barriers to care access have resulted in a lack of essential youth behavioral health care in New Hampshire. Over the past decade, there have been efforts across NH to address this through Behavioral Health Integration (BHI), from multi-year initiatives to practice-level training or self-funded quality improvement projects. Despite the best efforts of many, the resulting increase in service capacity has been extremely limited. In order to inform future work in BHI, this assessment compiles the experiences, thoughts, and beliefs of primary care professionals and payers pertaining to the current availability, delivery, and payment methodologies of behavioral health services in primary care.
National Oral Health Conference Poster
February 2015
With support from the Gary and Mary West Health Policy Center, the APCD Council has developed a manual for states to develop all-payer claims databases. The manual is a first of its-kind resource that provides states with detailed guidance on common data standards, collection, aggregation and analysis involved with establishing these databases.

May 2008-Present
The APCD Council is a learning collaborative of government, private, non-profit, and academic organizations focused on improving the development and deployment of state-based all payer claims databases(APCD). The Council's work focuses on shared learning amongst APCD stakeholders, early stage technical assistance to states and catalyzing states to achieve mutual goals.