The Institute for Health Policy and Practice's efforts in the area of Delivery System and Payment Reform drives healthcare systems change to improve healthcare quality and support value-based payment.
For more information, contact Janet Thomas at janet.thomas@unh.edu
NH Citizens Health Initiative Annual Symposium
Traversing Together: Finding Success in Chaos
The NH Citizens Health Initiative virtual 2022 Symposium reflected on the experiences of families, providers, organizations, and communities in the last few years, exacerbated by the challenges presented by the COVID-19 pandemic and highlighted the success and strategies utilized across sectors from an individual, organizational, state, and national perspective. We hope the sessions throughout the day provided you and your organization opportunities to share learning, to connect and to energize as we move forward health and health care for all in New Hampshire.
Projects and Initiatives

The mission of the NH Citizens Health Initiative is to measurably improve the systems that finance and provide health care in New Hampshire, by providing trusted leadership, data, and shared learning with the goal of achieving the quadruple aim: achieving better health outcomes, with a better patient care experience, at a lower cost, and with higher provider satisfaction.
The UNH Advanced Nursing Education Workforce (ANEW) program funds Primary Care Family Nurse Practitioner (NP) and Psychiatric Mental Health Nurse Practitioner students with trainee-ship awards to students who work and train in rural and under-served settings. ANEW provides NP students with the practice, preceptor, and peer support they need to address current workforce challenges in these unique primary care environments. ANEW also provides support and professional development opportunities for preceptors working alongside ANEW trainee-ship students.
ANEW professional development focuses on the key, high priority health concerns of rural New Hampshire, including behavioral health, substance use disorder, and telehealth providing continuing education for both the preceptor and NP preceptee using an all-teach all-learn continuing education strategy.
This grant is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $2.6 million dollars with a percentage financed with non-governmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement by HRSA, HHS, or the U.S. Government. For more information please visit HRSA.gov.
ANEW has also hosted three cohorts of the Preceptor ECHO® to Enhance Rotations (PEER) to help enhance the overall preceptor experience for students, preceptors, and support staff.
To learn more about the Preceptor ECHO to Enhance Rotations and to access additional resources, please click on the accordion sections below.
PEER Didactics
The Preceptor ECHO to Enhance Rotations (PEER) project promotes case-based shared learning across clinical preceptor sites throughout New England and beyond, developing a learning community of preceptors and practice sites while sharing and developing competencies for rural and under-served preceptor sites.
UNH Advanced Nursing Education Workforce Grant
LEARN MORE about the Advanced Nursing Education Workforce Grant
Preceptors Resources and Opportunities
UVM CORA

The University of Vermont Center on Rural Addiction (UVM CORA) is supported by the Health Resources Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS), and was established in the fall of 2019. Our mission is to expand addiction treatment capacity in rural communities by providing consultation, resources, training, and evidence-based technical assistance to healthcare providers and other staff. At UVM CORA, we want to leverage our expertise in evidence-based practices for treating Opioid Use Disorder (OUD) and other Substance Use Disorders (SUDs) to:
- Identify real-time needs of rural communities and science-supported methods for effectively addressing current and future addiction needs.
- Deliver ongoing technical assistance and workforce training to support the effective use of best practices for assessing and treating rural patients.
- Disseminate education and resources on evidence-based treatment and prevention to rural providers and policymakers.
Our priority areas cover the HRSA-designated rural counties in VT, NH, ME, and northern NY, but our Center is designed to provide services nationally.
COLLABORATIVE FOR ADVANCING RURAL EXCELLENCE AND EQUITY (CARE2)

The Collaborative for Advancing Rural Excellence and Equity (CARE2) aims to support health care providers who serve two populations that lack access to quality health care: older adults who are socially isolated, and adults and older adults with substance use disorder (SUD) and/or behavioral health needs.
The project described is supported by grant number U3IRH43508 from the Office for the Advancement of Telehealth, Health Resources and Services Administration, DHHS. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement by, HRSA/HHS or the U.S. Government. CARE2 is a collaboration between MCD Global Health and University of New Hampshire Institute for Health Policy and Practice.
NH Mental Health Access in Pediatrics (NH MCAP)

In collaboration with the NH Maternal Child Health Bureau, the NH Pediatric Improvement Partnership is conducting the NH Mental Health Access In Pediatrics (NH MCAP) Project. Funded by a multi-year Health Resources and Services Administration Cooperative Agreement, the goal of NH MCAP is to promote behavioral health integration in pediatric primary care by:1) training and supporting NH's health care providers to identify and care for children with pediatric mental health conditions; 2) enabling front-line health providers to receive provider teleconsultation services about the identification and treatment of children with a mental health condition; 3) enhancing the delivery of services through the creation of a referral directory of pediatric mental/behavioral health services and supports.

NH Pediatric Improvement Partnership
Started in 2013, the New Hampshire Pediatric Improvement Partnership (NHPIP) is a program of the NH Citizens Health Initiative, coordinated by the Institute for Health Policy and Practice at UNH, with Medical Director leadership from the Children's Hospital at Dartmouth (see graphic below). The NHPIP is a state-level multi-disciplinary collaborative of private and public partners dedicated to improving health care quality for all NH children through the use of systems and measurement-based quality improvement processes. We do this through:
- Promoting awareness of and interest in pediatric care quality measurement, projects, and resources
- Facilitating dialogue to identify and act upon pediatric care quality opportunities in NH.
- Conducting and/or collaborating on pediatric quality improvement projects
TRAUMA-INFORMED CARE IN PEDIATRICS

Funded by the NH Children’s Health Foundation, the NH Trauma-informed Care in Pediatrics Project is a 2.5 year project focused on increasing the capacity of NH pediatric primary care clinicians in screening for and responding to adverse childhood experiences (ACEs). ACEs are potentially traumatic events that occur during childhood such as physical emotional abuse, neglect, caregiver mental illness, and household violence. The goals of this NH Pediatric Improvement Partnership (NHPIP) project are to:
1) Increase pediatric general practitioner knowledge about trauma-informed care and existing tools to support addressing trauma in primary care settings and
2) Support five pediatric primary care clinics in using quality improvement principles to pilot process(es) to detect and respond to patients experiencing toxic stress.
The University of New Hampshire is a Project ECHO® Hub led by the NH Citizens Health Initiative, a program of the UNH Institute for Health Policy and Practice. The UNH Project ECHO Hub launched in 2018 and has developed learning communities on a range of topics. The goal of the UNH Project ECHO hub is to share knowledge and increase expertise throughout communities in New Hampshire, New England, and nationally.
Resources and Publications
September 2023
To improve access to behavioral health services in NH, we must expand the roles and settings that can effectively screen, assess, and treat children and adolescents with mild to moderate mental health conditions. Doing so would allow specialty behavioral health providers, an already limited resource, to focus on patients with severe or complex clinical needs. Both the Collaborative Care (CoCM) and Child Psychiatric Access Program (Access Program) models of care have been shown to improve access to behavioral health care while optimizing use of the limited workforce of child and adolescent psychiatrists (CAPs).
Mental Health Care Access for NH Youth: A Comparison of Two Models
September 2023
A shortage of specialty providers and numerous barriers to care access have resulted in a lack of essential youth behavioral health care in New Hampshire. Over the past decade, there have been efforts across NH to address this through Behavioral Health Integration (BHI), from multi-year initiatives to practice-level training or self-funded quality improvement projects. Despite the best efforts of many, the resulting increase in service capacity has been extremely limited. In order to inform future work in BHI, this assessment compiles the experiences, thoughts, and beliefs of primary care professionals and payers pertaining to the current availability, delivery, and payment methodologies of behavioral health services in primary care.
The Current State of Behavioral Health in Primary Care for NH Youth

August 2023
The Collaborative for Advancing Rural Excellence and Equity (CARE2) is a federally funded five-year program with the UNH ECHO Hub in collaboration with our partners, MCD Global Health, to provide two Project ECHO series annually on the topics of aging and substance use to care teams in New Hampshire, Maine, Vermont, and North Country New York. The Annual Report Evaluation Highlights from CARE2 Project Year 1 was developed to serve as a quantitative and qualitative review of our program’s impact across Cohort 1 of both of our ECHO programs: Project ECHO: Aging, Community, & Equity and the Substance Use Disorder (SUD) ECHO.
Collaborative for Advancing Rural Excellence and Equity (CARE2) Annual Report: Evaluation Highlights

June 2023
Background/Aims Community mental health centres in the US often struggle to implement the evidenced-based metrics and measurement processes required for quality reporting initiatives. Through the co-design and facilitation of a learning collaborative, all 10 community mental health centres in New Hampshire agreed on the goal of demonstrating measurement alignment and improvement across three behavioural health metrics related to depression and suicide risk, aiming for a screening rate of at least 85% in a year.
Methods The learning system framework and Lean Six Sigma define, measure, analyse, improve and control methodologies were used to increase participation and improve quality reporting. Teams were asked to participate in both a group learning collaborative and individual centre facilitation sessions, working with a quality improvement specialist. Reported measures were compared with subsets of the population data and between centres. Outliers were identified for potential reporting inaccuracies and opportunities for improvement.
Results All 10 community mental health centres were able to accurately report screening results on all three measures. After 12 months, 70% of the teams were able to reach the group-determined goal of at least 85% of eligible patients being screened in one measure, 40% of the teams met the benchmark in two measures and 20% of the teams were able to meet the benchmark in all three measures.
Conclusions Early investment by community mental health centre leadership through the development of a shared aim and project outcomes is essential to support learning and achieve positive outcomes. Quality improvement specialists are vital for facilitation of shared learning and practice across organisations.
September 2023
Investing in Primary Care: Advancing Nursing Education Workforce
December 2022
In April of 2022, the Institute for Health Policy and Practice (IHPP), in collaboration with the Department of Health and Human Services (DHHS) and the NH Pediatric Improvement Partnership (NH PIP), published the first version of the Mental Health Care Access in Pediatrics (MCAP) report, New Hampshire Children and Teens Experiencing Mental Health Disorders: An Analysis of 2019 Healthcare Claims Data. This report builds on the work of that publication, providing an analysis that explores care patterns in 2020, at the beginning of the 2020 COVID-19 pandemic. This update also includes an additional section focused on the providers of mental health care based on medical and pharmaceutical claims data.
August 2022
The Chronic Pain Self-Management ECHO was formed to provide educational content and a networking opportunity for those in rural New Hampshire and New England who work with individuals with chronic pain. This opportunity was in collaboration with the NH Citizens Health Initiative at the UNH Institute for Health Policy and Practice and the UNH Extension team. Six sessions were offered from September 2021 to March 2022. This evaluation report highlights the program background, participation in the series, impact of the series on participants, and considers future opportunities for education, research, and training on the topic of chronic pain self-management. Additional findings will be forthcoming.
Chronic Pain Self-Management Project ECHO Series: Evaluation Highlights

April 2022
The NH Mental Health Care Access in Pediatrics (MCAP) program is a collaborative effort of the NH Department of Health and Human Services and the NH Pediatric Improvement Partnership housed at the UNH Institute for Health Policy and Practice. Funded by the Health Resources and Services Administration, the focus of MCAP is to promote behavioral health integration in pediatric primary care. MCAP provides 1) training to pediatric and family practice clinicians in assessing and treating common pediatric mental health conditions through an annual Project ECHO® learning series, 2) clinician-to-clinician teleconsultation services, and 3) an annually updated referral directory of pediatric mental/behavioral health services in New Hampshire. To inform its programming, MCAP funded this analysis of 2019 pediatric medical and pharmacy claims data from commercial and NH Medicaid payers. Specifically, MCAP sought to examine health care claims for NH’s pediatric population to provide a descriptive analysis of:
- The burden of pediatric mental health conditions as defined by the percentage of children under age 18 with mental health conditions,
- Mental health conditions and comorbidities with other mental health conditions, and
- Mental health medical and pharmaceutical service utilization to produce measures of treatment.
April 2022
The purpose of this handbook is to guide pediatric and family practice primary care clinics and/or quality improvement (QI) organizations to initiate a process to screen for and respond to Adverse Childhood Experiences (ACEs). This handbook is based on the experience of the New Hampshire Pediatric Improvement Partnership (NH PIP) in supporting five New Hampshire pediatric practices in developing and piloting workflows to address ACEs within their patient population. The handbook provides a short background on project need, followed by a description of the initial implementation plan and required modifications due to varied factors. Next, this handbook outlines the results and lessons learned from of the project’s process evaluation. Finally, the handbook concludes with an improved and updated description of this QI process for replication elsewhere.
Facilitating a Quality Improvement Approach to Childhood Adversity Screening in Primary Care: A Handbook, owned by the University of New Hampshire and authored by Felicity Bernard, Corina Chao, Holly Tutko, and Dee Watts, licensed under CC BY NC ND 2.0.
April 2022
The purpose of this document is to serve as a practical guide to implementing trauma-informed care practices in Pediatric primary care clinics. It is designed to provide structure to the processes that are recommended to successfully, detect, treat and provide referrals to families who have experienced trauma and to build capacity and competence for a busy primary care office.
A Guide to Trauma-Informed Pediatric Primary Care, owned by the University of New Hampshire and authored by Felicity Bernard, Corina Chao, Holly Tutko, and Dee Watts, licensed under CC BY NC ND 2.0.

March 2022
Improving Pediatric Mental Health in NH through Collaboration and Community
March 2022
Pediatric Trauma-Informed Care at Various Levels of Integration
February 2022
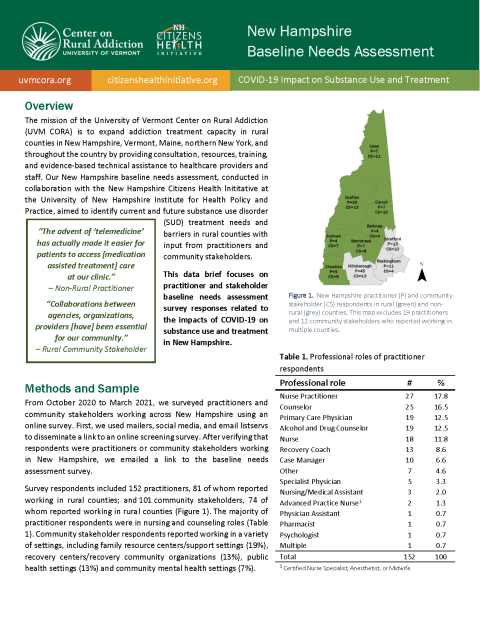
The mission of the University of Vermont Center on Rural Addiction (UVM CORA) is to expand addiction treatment capacity in rural counties by providing consultation, resources, training, and evidence-based technical assistance to healthcare practitioners and other staff. With the baseline needs assessment, UVM CORA aims to identify current and future addiction treatment needs and barriers in New Hampshire with direct input from practitioners, policymakers, and other stakeholders.
August 2021
This data brief focuses on practitioner and stakeholder baseline needs assessment survey responses related to the impacts of COVID-19 on substance use and treatment in New Hampshire.
UVM CORA NH BNA COVID-19 Impact on Substance Use and Treatment Data Brief
October 2020
Teleprecepting grants us the opportunity to continue to lead the next generation of providers in caring for patients across the care continuum. Regardless of whether telehealth is being used as an emergency stopgap or will become a tool for ongoing practice, we must not delay in leading the next generation of providers and incorporating students into the care continuum.
March 2020
Project Extension for Community Healthcare Outcomes (ECHO)is an evidence-based method using web-based teleconferencing to link specialist teams with community-based sites to help community providers improve their ability to manage complex conditions. It has been proven to improve health care outcomes for vulnerable populations with limited access to care because of socioeconomic factors or geography. The New Hampshire Project ECHO Planning for Implementation and Business Sustainability Project undertook a planning process to inform how to best develop Project ECHO at UNH to serve New Hampshire health and community care providers and ultimately improve access to effective, timely care. Also included is a business and sustainability plan for long-term success of the UNH Project ECHO Hub and an evaluation plan for measuring efficacy.
March 2020
In 10 Steps for Improving Diabetes Care in New Hampshire you will find an easy-to-follow stepwise format of practical, best-practice strategies that are feasible to implement in any primary care setting. These Strategies are applicable to planning for prediabetes, as well.
July 2020
The Endowment for Health and SPARK NH funded the NH Pediatric Improvement Partnership to develop a set of recommendations to address identifying and responding to Adverse Childhood Experiences and Social Determinants of Health in NH primary care settings caring for children. Methods included conducting a review of literature and Key Informant Interviews. Themes from these were identified and the findings are summarized in this report.