IHPP Publications
September 2023
To improve access to behavioral health services in NH, we must expand the roles and settings that can effectively screen, assess, and treat children and adolescents with mild to moderate mental health conditions. Doing so would allow specialty behavioral health providers, an already limited resource, to focus on patients with severe or complex clinical needs. Both the Collaborative Care (CoCM) and Child Psychiatric Access Program (Access Program) models of care have been shown to improve access to behavioral health care while optimizing use of the limited workforce of child and adolescent psychiatrists (CAPs).
Mental Health Care Access for NH Youth: A Comparison of Two Models
September 2023
A shortage of specialty providers and numerous barriers to care access have resulted in a lack of essential youth behavioral health care in New Hampshire. Over the past decade, there have been efforts across NH to address this through Behavioral Health Integration (BHI), from multi-year initiatives to practice-level training or self-funded quality improvement projects. Despite the best efforts of many, the resulting increase in service capacity has been extremely limited. In order to inform future work in BHI, this assessment compiles the experiences, thoughts, and beliefs of primary care professionals and payers pertaining to the current availability, delivery, and payment methodologies of behavioral health services in primary care.
The Current State of Behavioral Health in Primary Care for NH Youth

August 2023
The Collaborative for Advancing Rural Excellence and Equity (CARE2) is a federally funded five-year program with the UNH ECHO Hub in collaboration with our partners, MCD Global Health, to provide two Project ECHO series annually on the topics of aging and substance use to care teams in New Hampshire, Maine, Vermont, and North Country New York. The Annual Report Evaluation Highlights from CARE2 Project Year 1 was developed to serve as a quantitative and qualitative review of our program’s impact across Cohort 1 of both of our ECHO programs: Project ECHO: Aging, Community, & Equity and the Substance Use Disorder (SUD) ECHO.
Collaborative for Advancing Rural Excellence and Equity (CARE2) Annual Report: Evaluation Highlights

June 2023
Background/Aims Community mental health centres in the US often struggle to implement the evidenced-based metrics and measurement processes required for quality reporting initiatives. Through the co-design and facilitation of a learning collaborative, all 10 community mental health centres in New Hampshire agreed on the goal of demonstrating measurement alignment and improvement across three behavioural health metrics related to depression and suicide risk, aiming for a screening rate of at least 85% in a year.
Methods The learning system framework and Lean Six Sigma define, measure, analyse, improve and control methodologies were used to increase participation and improve quality reporting. Teams were asked to participate in both a group learning collaborative and individual centre facilitation sessions, working with a quality improvement specialist. Reported measures were compared with subsets of the population data and between centres. Outliers were identified for potential reporting inaccuracies and opportunities for improvement.
Results All 10 community mental health centres were able to accurately report screening results on all three measures. After 12 months, 70% of the teams were able to reach the group-determined goal of at least 85% of eligible patients being screened in one measure, 40% of the teams met the benchmark in two measures and 20% of the teams were able to meet the benchmark in all three measures.
Conclusions Early investment by community mental health centre leadership through the development of a shared aim and project outcomes is essential to support learning and achieve positive outcomes. Quality improvement specialists are vital for facilitation of shared learning and practice across organisations.
September 2023
Investing in Primary Care: Advancing Nursing Education Workforce
December 2022
In April of 2022, the Institute for Health Policy and Practice (IHPP), in collaboration with the Department of Health and Human Services (DHHS) and the NH Pediatric Improvement Partnership (NH PIP), published the first version of the Mental Health Care Access in Pediatrics (MCAP) report, New Hampshire Children and Teens Experiencing Mental Health Disorders: An Analysis of 2019 Healthcare Claims Data. This report builds on the work of that publication, providing an analysis that explores care patterns in 2020, at the beginning of the 2020 COVID-19 pandemic. This update also includes an additional section focused on the providers of mental health care based on medical and pharmaceutical claims data.
August 2022
The Chronic Pain Self-Management ECHO was formed to provide educational content and a networking opportunity for those in rural New Hampshire and New England who work with individuals with chronic pain. This opportunity was in collaboration with the NH Citizens Health Initiative at the UNH Institute for Health Policy and Practice and the UNH Extension team. Six sessions were offered from September 2021 to March 2022. This evaluation report highlights the program background, participation in the series, impact of the series on participants, and considers future opportunities for education, research, and training on the topic of chronic pain self-management. Additional findings will be forthcoming.
Chronic Pain Self-Management Project ECHO Series: Evaluation Highlights

April 2022
The NH Mental Health Care Access in Pediatrics (MCAP) program is a collaborative effort of the NH Department of Health and Human Services and the NH Pediatric Improvement Partnership housed at the UNH Institute for Health Policy and Practice. Funded by the Health Resources and Services Administration, the focus of MCAP is to promote behavioral health integration in pediatric primary care. MCAP provides 1) training to pediatric and family practice clinicians in assessing and treating common pediatric mental health conditions through an annual Project ECHO® learning series, 2) clinician-to-clinician teleconsultation services, and 3) an annually updated referral directory of pediatric mental/behavioral health services in New Hampshire. To inform its programming, MCAP funded this analysis of 2019 pediatric medical and pharmacy claims data from commercial and NH Medicaid payers. Specifically, MCAP sought to examine health care claims for NH’s pediatric population to provide a descriptive analysis of:
- The burden of pediatric mental health conditions as defined by the percentage of children under age 18 with mental health conditions,
- Mental health conditions and comorbidities with other mental health conditions, and
- Mental health medical and pharmaceutical service utilization to produce measures of treatment.
April 2022
The purpose of this handbook is to guide pediatric and family practice primary care clinics and/or quality improvement (QI) organizations to initiate a process to screen for and respond to Adverse Childhood Experiences (ACEs). This handbook is based on the experience of the New Hampshire Pediatric Improvement Partnership (NH PIP) in supporting five New Hampshire pediatric practices in developing and piloting workflows to address ACEs within their patient population. The handbook provides a short background on project need, followed by a description of the initial implementation plan and required modifications due to varied factors. Next, this handbook outlines the results and lessons learned from of the project’s process evaluation. Finally, the handbook concludes with an improved and updated description of this QI process for replication elsewhere.
Facilitating a Quality Improvement Approach to Childhood Adversity Screening in Primary Care: A Handbook, owned by the University of New Hampshire and authored by Felicity Bernard, Corina Chao, Holly Tutko, and Dee Watts, licensed under CC BY NC ND 2.0.
April 2022
The purpose of this document is to serve as a practical guide to implementing trauma-informed care practices in Pediatric primary care clinics. It is designed to provide structure to the processes that are recommended to successfully, detect, treat and provide referrals to families who have experienced trauma and to build capacity and competence for a busy primary care office.
A Guide to Trauma-Informed Pediatric Primary Care, owned by the University of New Hampshire and authored by Felicity Bernard, Corina Chao, Holly Tutko, and Dee Watts, licensed under CC BY NC ND 2.0.

March 2022
Improving Pediatric Mental Health in NH through Collaboration and Community
March 2022
Pediatric Trauma-Informed Care at Various Levels of Integration
February 2022
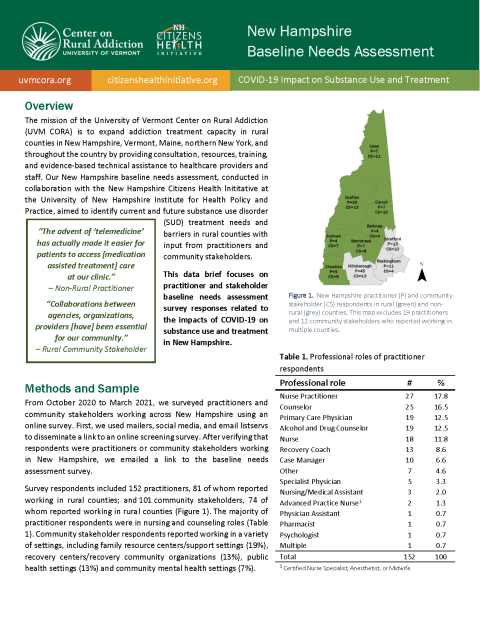
The mission of the University of Vermont Center on Rural Addiction (UVM CORA) is to expand addiction treatment capacity in rural counties by providing consultation, resources, training, and evidence-based technical assistance to healthcare practitioners and other staff. With the baseline needs assessment, UVM CORA aims to identify current and future addiction treatment needs and barriers in New Hampshire with direct input from practitioners, policymakers, and other stakeholders.
August 2021
This data brief focuses on practitioner and stakeholder baseline needs assessment survey responses related to the impacts of COVID-19 on substance use and treatment in New Hampshire.
UVM CORA NH BNA COVID-19 Impact on Substance Use and Treatment Data Brief
October 2020
Teleprecepting grants us the opportunity to continue to lead the next generation of providers in caring for patients across the care continuum. Regardless of whether telehealth is being used as an emergency stopgap or will become a tool for ongoing practice, we must not delay in leading the next generation of providers and incorporating students into the care continuum.
March 2020
Project Extension for Community Healthcare Outcomes (ECHO)is an evidence-based method using web-based teleconferencing to link specialist teams with community-based sites to help community providers improve their ability to manage complex conditions. It has been proven to improve health care outcomes for vulnerable populations with limited access to care because of socioeconomic factors or geography. The New Hampshire Project ECHO Planning for Implementation and Business Sustainability Project undertook a planning process to inform how to best develop Project ECHO at UNH to serve New Hampshire health and community care providers and ultimately improve access to effective, timely care. Also included is a business and sustainability plan for long-term success of the UNH Project ECHO Hub and an evaluation plan for measuring efficacy.
March 2020
In 10 Steps for Improving Diabetes Care in New Hampshire you will find an easy-to-follow stepwise format of practical, best-practice strategies that are feasible to implement in any primary care setting. These Strategies are applicable to planning for prediabetes, as well.
July 2020
The Endowment for Health and SPARK NH funded the NH Pediatric Improvement Partnership to develop a set of recommendations to address identifying and responding to Adverse Childhood Experiences and Social Determinants of Health in NH primary care settings caring for children. Methods included conducting a review of literature and Key Informant Interviews. Themes from these were identified and the findings are summarized in this report.

Covering the Care: Pregnancy Tops the List of Highest Out-Of-Pocket Costs for NH’s Commercially Insured
February 2025
This data brief presents a retrospective analysis of available medical claims data from New Hampshire’s commercial insurance plans. This brief focuses on conditions with the highest average out-of-pocket costs paid by commercially insured members in 2022. It also examines how out-of-pocket costs for those conditions have changed over a seven-year period (2016-2022). The analysis is based on claims data from January 2016 – December 2022 and is analyzed at the overall population level and by member gender. It is part of a series of analytic briefs examining the rate of the most common health conditions and treatment costs for those respective conditions.

Covering the Care: Pharmaceutical Utilization and Per-Member-Per-Month Costs
January 2025
This data brief presents a retrospective descriptive analysis of pharmaceutical utilization and its associated costs by utilizing available pharmacy claims data from three of New Hampshire’s insurance payers: commercial, NH Medicaid, and NH Medicare. The brief identifies the top ten drug classes by number of prescriptions filled and their per-member-per-month costs. The analysis is based on the most recent calendar year of pharmacy claims data available (January – December 2022).
Covering the Care: Pharmaceutical Utilization and Per-Member-Per-Month Costs

Covering the Care: Most Costly Health Conditions – Metabolic Disorders, Hemophilia, Cancers, and Transplants Top the List
February 2025
This data brief presents a retrospective analysis of available medical claims data from New Hampshire’s commercial, Medicaid, and Medicare insurance programs. This brief focuses on the conditions that incur the highest medical costs, regardless of their prevalence among the population. Metabolic disorders, hemophilia, certain cancers, and transplants were identified across all three payers as some of the costliest conditions. Most of these conditions have low prevalence and could, in some instances, be considered rare. There is variability in the prevalence of these conditions by payer type and there is a variability in the costs paid by payer type, with commercial insurance consistently having the highest costs. The analysis uses administrative medical claims data from January to December 2022.
Assessment Tools for Evaluating Primary Care Services and Delivery from the Consumer and Provider Perspective
February 2024
Develop a synthesis of tools and recommendations for collecting data from patients and clinicians related to primary care services and care delivery. Create a report of recommended tools that have been used and validated, ideally with an appendix of the actual survey instruments when they are available and can be used either with permission or for a fee.
February 2024
As a part of the Endowment for Health’s comprehensive strategy to improve the health of the people in New Hampshire (NH), the foundation invests in the University of New Hampshire Institute for Health Policy and Practice Health (UNH IHPP) to research and inform statewide health law and policy. Specifically, funding in 2023 focused on the provision of primary care in NH, which IHPP addressed through two reports and a focus group. The reports included a landscape on existing best-practice literature in primary care and, a review of assessment tools for evaluating primary care services and delivery. This paper provides a summary and findings of the focus group.
September 2023
A shortage of specialty providers and numerous barriers to care access have resulted in a lack of essential youth behavioral health care in New Hampshire. Over the past decade, there have been efforts across NH to address this through Behavioral Health Integration (BHI), from multi-year initiatives to practice-level training or self-funded quality improvement projects. Despite the best efforts of many, the resulting increase in service capacity has been extremely limited. In order to inform future work in BHI, this assessment compiles the experiences, thoughts, and beliefs of primary care professionals and payers pertaining to the current availability, delivery, and payment methodologies of behavioral health services in primary care.
The Current State of Behavioral Health in Primary Care for NH Youth Report
September 2023
Investing in Primary Care: Advancing Nursing Education Workforce
September 2023
NH Children and Teens Experiencing Mental Health Disorders: An Analysis of 2019-2021 Health Care Claims Data
April 2023
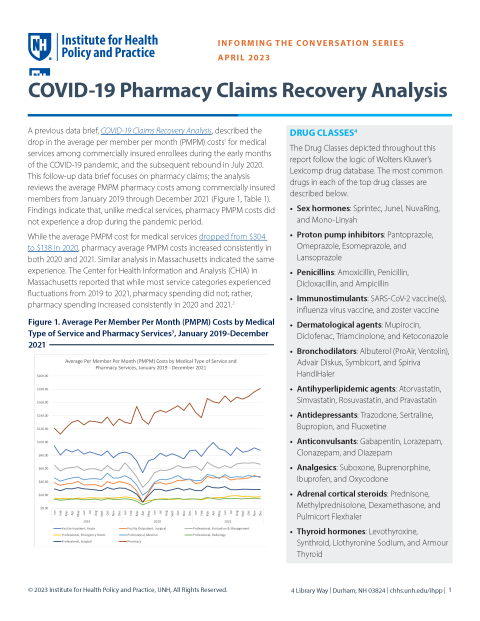
COVID-19 Pharmacy Claims Recovery Analysis
January 2023
COVID-19 Claims Recovery Analysis
December 2022
In April of 2022, the Institute for Health Policy and Practice (IHPP), in collaboration with the Department of Health and Human Services (DHHS) and the NH Pediatric Improvement Partnership (NH PIP), published the first version of the Mental Health Care Access in Pediatrics (MCAP) report, New Hampshire Children and Teens Experiencing Mental Health Disorders: An Analysis of 2019 Healthcare Claims Data. This report builds on the work of that publication, providing an analysis that explores care patterns in 2020, at the beginning of the 2020 COVID-19 pandemic. This update also includes an additional section focused on the providers of mental health care based on medical and pharmaceutical claims data.
New Hampshire Child and Teen Mental Health: An Analysis and Comparison of 2019-2020 Healthcare Claims Data

April 2022
The NH Mental Health Care Access in Pediatrics (MCAP) program is a collaborative effort of the NH Department of Health and Human Services and the NH Pediatric Improvement Partnership housed at the UNH Institute for Health Policy and Practice. Funded by the Health Resources and Services Administration, the focus of MCAP is to promote behavioral health integration in pediatric primary care. MCAP provides: 1) training to pediatric and family practice clinicians in assessing and treating common pediatric mental health conditions through an annual Project ECHO® learning series, 2) clinician-to-clinician teleconsultation services, and 3) an annually updated referral directory of pediatric mental/behavioral health services in New Hampshire. To inform its programming, MCAP funded this analysis of 2019 pediatric medical and pharmacy claims data from commercial and NH Medicaid payers. Specifically, MCAP sought to examine health care claims for NH’s pediatric population to provide a descriptive analysis of:
- The burden of pediatric mental health conditions as defined by the percentage of children under age 18 with mental health conditions,
- Mental health conditions and comorbidities with other mental health conditions, and
- Mental health medical and pharmaceutical service utilization to produce measures of treatment.
August 2021
The Center for Health Analytics, with funding from the Children's Health Foundation, has published their oral health report which analyzes dental claims to understand patterns of oral health care services, in addition to use of fluoride and patterns of care during the COVID-19 pandemic.
March 2021
The Center for Health Analytics (CHA) at the Institute for Health Policy and Practice (IHPP) has released a new report, Cost and Utilization of Treatment for Diabetes in New Hampshire: Analysis of Medical and Pharmacy All-Payer Claims Data. By utilizing tables from IHPP's NH Claims Report Suite, CHA analyzed measures of cost and utilization for Commercial (NHCHIS), NH Medicaid and NH Medicare beneficiaries who are indicated to have diabetes and/or the related heart conditions of Congestive Heart Failure, Hypertension and Cardiovascular Disease. This report includes an overview of how diabetes and the selected heart conditions compare to the 20 most common conditions for each payer population as well as a comparison of costs and utilization of drugs classified as anti-diabetic agents to the top 10 drug classes by total scripts. The report also analyzes variations of costs for beneficiaries with diabetes or the selected heart conditions with and without co-morbidities. This project was funded by the Division of Public Health Services at NH Department of Health and Human Services.
June 2020
The Institute for Health Policy and Practice, leveraging the UNH Survey Center's Granite State Panel, conducted a survey of NH adults to understand some of the immediate impacts of COVID-19 since January 2020. The survey includes 1155 respondents, and was fielded from April 16-20, 2020.

2020
To better understand a broad range of issues related to the cost and utilization of health care services, IHPP maintains a suite of analytic reports based on NH medical, pharmacy and dental claims data. The NH Claims Report Suite contains measures of types of service, burden of specific diseases and conditions, and use of medications, with the ability to drill down by population and geographic characteristics. This work was funded with support from the Endowment for Health and the New Hampshire Children's Health Foundation. For more information about the data sources, please see the methods tabs within the report suite. To learn more about the commercial claims data, visit nhchis.org.
2017
A shortage of specialty providers and numerous barriers to care access have resulted in a lack of essential youth behavioral health care in New Hampshire. Over the past decade, there have been efforts across NH to address this through Behavioral Health Integration (BHI), from multi-year initiatives to practice-level training or self-funded quality improvement projects. Despite the best efforts of many, the resulting increase in service capacity has been extremely limited. In order to inform future work in BHI, this assessment compiles the experiences, thoughts, and beliefs of primary care professionals and payers pertaining to the current availability, delivery, and payment methodologies of behavioral health services in primary care.
National Oral Health Conference Poster
February 2015
With support from the Gary and Mary West Health Policy Center, the APCD Council has developed a manual for states to develop all-payer claims databases. The manual is a first of its-kind resource that provides states with detailed guidance on common data standards, collection, aggregation and analysis involved with establishing these databases.

May 2008-Present
The APCD Council is a learning collaborative of government, private, non-profit, and academic organizations focused on improving the development and deployment of state-based all payer claims databases(APCD). The Council's work focuses on shared learning amongst APCD stakeholders, early stage technical assistance to states and catalyzing states to achieve mutual goals.

Covering the Care: Chronic conditions, including behavioral health, drive a significant proportion of high-utilizer emergency department visits in 2023.
January 2026
This data brief summarizes a retrospective analysis of commercial, New Hampshire Medicaid, and New Hampshire Medicare claims, examining common reasons for emergency department visits among children aged 0-18, adults aged 19-44, adults aged 45-64, and adults aged 65 years and older in calendar year 202

Covering the Care: The Fourth Trimester
January 2026
The weeks following the birth of a baby are often described as a time of extremes: profound joy paired with deep exhaustion, vulnerability, and adjustment. For birthing people, this period involves physical recovery from childbirth, dramatic hormonal shifts, disrupted sleep, learning to feed and care for an infant, and navigating major emotional changes. While some new parents have strong support systems, others face isolation, housing instability, or unsafe home environments. This critical 12-week period after birth is now widely known as the “fourth trimester.” Although the language is new, the reality is not. Across cultures and history, the postpartum period has been recognized as a time requiring focused care for both mother and baby. Yet within the U.S. medical system, postpartum support remains strikingly limited.

Covering the Care: Medical Debt: A Uniquely American Issue
January 2026
Healthcare is one of the most prominent issues facing Americans due to issues of affordability, access, and potential for debt. A July 2025 poll from Kaiser Family Foundation indicates that approximately half of U.S. adults say it is difficult to afford healthcare costs and about one third of adults say they have postponed care in the last year because of the cost. According to a 2024 New Hampshire specific survey, 69% of adults have delayed or gone without healthcare due to cost, 71% of adults have experienced a healthcare affordability issue in the past year, and more than 80% worry about affording healthcare in the future.
These healthcare affordability concerns are not limited to those who are uninsured. Six in ten insured adults worry about affording out-of-pocket costs not covered by insurance, such as co-pays and deductibles. Unexpected healthcare costs are a primary contributor to medical debt.

Covering the Care: Why Financial Resources Matter for Health
January 2026
Where people end up in the income and wealth distribution has a powerful and lasting influence on how healthy they are and how long they live. This is not just a story about poverty versus comfort. Across the entire population, health improves step by step as financial resources increase. Researchers call this pattern the health gradient.
This brief explains why that gradient exists. Drawing on decades of research from economics, public health, and social epidemiology, it shows how limited financial resources shape health through multiple pathways that unfold over different time horizons—from immediate consequences to cumulative effects that build over a lifetime.
Covering the Care: Why Financial Resources Matter for Health

Covering the Care: Utilization Rate Trends Among NH Older Adults Enrolled in Medicare Aged 65 and Over
January 2026
This data brief summarizes a retrospective analysis of New Hampshire Medicare Parts A and B claims, examining six-year (2018–2023) trends in utilization rates for selected medical services among adults aged 65 and older. It is the third and last of a three-part series of Covering the Care analytic reports exploring healthcare utilization trends in the state.
Covering the Care: Utilization Rate Trends Among Children Ages 0-18
December 2025
This data brief provides a retrospective analysis of medical claims from NH Medicaid and commercial insurers, examining trends in utilization rates for selected medical services among children ages 0–18 over a six-year period (2018–2023).1 It is the second of a three-part series of Covering the Care analytic reports exploring healthcare utilization trends in New Hampshire.
Covering the Care: Utilization Rate Trends Among Children Ages 0-18

Covering the Care: Utilization Rate Trends Among NH Older Adults Enrolled in Medicare Aged 65 and Over
January 2026
This data brief summarizes a retrospective analysis of New Hampshire Medicare Parts A and B claims, examining six-year (2018–2023) trends in utilization rates for selected medical services among adults aged 65 and older. It is the third and last of a three-part series of Covering the Care analytic reports exploring healthcare utilization trends in the state.
Covering the Care: Utilization Rate Trends Among Children Ages 0-18
December 2025
This data brief provides a retrospective analysis of medical claims from NH Medicaid and commercial insurers, examining trends in utilization rates for selected medical services among children ages 0–18 over a six-year period (2018–2023).1 It is the second of a three-part series of Covering the Care analytic reports exploring healthcare utilization trends in New Hampshire.
Covering the Care: Utilization Rate Trends Among Children Ages 0-18

Covering the Care: Utilization Rate Trends Among Adults Ages 19-64
November 2025
This data brief presents a retrospective analysis of available medical claims data from NH Medicaid, NH Medicare and commercial insurance plans focusing on the trends of utilization rates for chosen medical interactions over a six-year period (2018-2023) among adults ages 19 to 64. This brief is the first of a three-part series of Covering the Care analytic reports exploring healthcare utilization trends in New Hampshire.
Covering the Care: Utilization Rate Trends Among Adults Ages 19-64
Covering the Care: Impacts of Labor and Delivery Unit Closures on Maternal Health Outcomes
2025
In 2022, more than half of rural hospitals and one-third of urban hospitals in the United States lacked obstetric services, reflecting an escalating trend of hospital labor and delivery (L&D) unit closures across the US. Despite some large-scale studies reporting negligible impacts of L&D closures on maternal health, an analysis of the literature presents a clear net-negative impact for vulnerable women, including those who identify as members of a racial or ethnic minority, those who have low-income, and those who are Medicaid members. For many families, the disappearance of local obstetric care is not merely an inconvenience but instead is a direct threat to health and safety, presenting as a reduction in access to care through pregnancy, an increase in travel-related risks, and potential life-threatening health outcomes.
Covering the Care: Impacts of Labor and Delivery Unit Closures on Maternal Health Outcomes

November 2025
The Institute for Health Policy and Practice (IHPP) of the University System of New Hampshire (USNH) contracted with Sarah Mason Eck of Scientific Health to provide evidence-based research on the effects of involvement in the criminal justice system with health outcomes.
The primary goal of this assignment was to identify, research, and review peer-reviewed, primary academic literature on studies examining how involvement with the correctional system impacts health outcomes.
Covering the Care: Hospital Consolidations Lead to Higher Healthcare Costs
October 2025
Time and time again, polls indicate that Americans are concerned about the cost of healthcare. It is one of the most prominent issues facing Americans because of affordability, access, and potential for debt. A July 2025 poll from Kaiser Family Foundation indicates that approximately half of U.S. adults say it is difficult to afford healthcare costs and about one third of adults say they have postponed care in the last year because of the cost. These concerns are not limited to those in the uninsured population; six in ten adults are worried about affording out-of-pocket costs not covered by insurance, such as co-pays and deductibles.
At the state level, according to a 2024 survey of New Hampshire adults, 71% have experienced a healthcare affordability issue in the past year, more than 80% worry about affording healthcare in the future, and 69% have delayed or gone without healthcare due to cost.
This is unsurprising given that the U.S. spends twice as much on healthcare than other wealthy countries in the world, yet has worse health outcomes. The high cost of healthcare can be attributed to a variety of factors, including high administrative costs, pharmaceutical pricing, fee-for-service care delivery, and lack of price regulation, among other factors. Over the past few decades, the U.S. has also experienced an acceleration of another contributing factor: healthcare consolidation. Data indicates that healthcare consolidations are linked to an increase in healthcare costs, often without improving the quality of care. These consolidations can also negatively impact access to healthcare in New Hampshire and across the country.
Covering the Care: Hospital Consolidations Lead to Higher Healthcare Costs

Covering the Care: Pregnancy Tops the List of Highest Out-Of-Pocket Costs for NH’s Commercially Insured
February 2025
This data brief presents a retrospective analysis of available medical claims data from New Hampshire’s commercial insurance plans. This brief focuses on conditions with the highest average out-of-pocket costs paid by commercially insured members in 2022. It also examines how out-of-pocket costs for those conditions have changed over a seven-year period (2016-2022). The analysis is based on claims data from January 2016 – December 2022 and is analyzed at the overall population level and by member gender. It is part of a series of analytic briefs examining the rate of the most common health conditions and treatment costs for those respective conditions.

Covering the Care: Most Costly Health Conditions – Metabolic Disorders, Hemophilia, Cancers, and Transplants Top the List
February 2025
This data brief presents a retrospective analysis of available medical claims data from New Hampshire’s commercial, Medicaid, and Medicare insurance programs. This brief focuses on the conditions that incur the highest medical costs, regardless of their prevalence among the population. Metabolic disorders, hemophilia, certain cancers, and transplants were identified across all three payers as some of the costliest conditions. Most of these conditions have low prevalence and could, in some instances, be considered rare. There is variability in the prevalence of these conditions by payer type and there is a variability in the costs paid by payer type, with commercial insurance consistently having the highest costs. The analysis uses administrative medical claims data from January to December 2022.

Covering the Care: Pharmaceutical Utilization and Per-Member-Per-Month Costs
January 2025
This data brief presents a retrospective descriptive analysis of pharmaceutical utilization and its associated costs by utilizing available pharmacy claims data from three of New Hampshire’s insurance payers: commercial, NH Medicaid, and NH Medicare. The brief identifies the top ten drug classes by number of prescriptions filled and their per-member-per-month costs. The analysis is based on the most recent calendar year of pharmacy claims data available (January – December 2022).
Covering the Care: Pharmaceutical Utilization and Per-Member-Per-Month Costs
August 2024
This data brief presents an analysis of available claims data from New Hampshire’s commercial, Medicaid, and Medicare insured populations. Specifically, the study identifies the top ten most prevalent health conditions, the cost of treatment for those conditions, and the overall medical cost for those with one of the identified conditions. The analysis is based on the most recent calendar year of available claims data (January – December 2022).
February 2024
The Institute for Health Policy and Practice (IHPP) of the College of Health and Human Services at the University of New Hampshire (UNH) contracted with Sarah Mason Eck of Scientific Health to provide a review of existing New Hampshire (NH) assessments and reports surrounding practices in primary care.
The primary goals of this assignment were to:
1. Review and synthesize data from within existing state, regional, and national assessments and reports regarding primary care and capacity in NH with a particular focus on infrastructure, access (barriers and utilization), clinical quality measures, provider workforce, and payment systems.
2. Review the literature for evidence-based best practices in primary health care, with a focus on primary care delivery models, payment methods, and spending measurement.
The State of Primary Care and Primary Care Capacity in New Hampshire
February 2024
As a part of the Endowment for Health’s comprehensive strategy to improve the health of the people in New Hampshire (NH), the foundation invests in the University of New Hampshire Institute for Health Policy and Practice Health (UNH IHPP) to research and inform statewide health law and policy. Specifically, funding in 2023 focused on the provision of primary care in NH, which IHPP addressed through two reports and a focus group. The reports included a landscape on existing best-practice literature in primary care and, a review of assessment tools for evaluating primary care services and delivery. This paper provides a summary and findings of the focus group.
Primary Care in New Hampshire Focus Group Report

July 2023
The UNH Franklin Pierce School of Law, Institute for Health Policy and Practice in collaboration with New Futures released the 2023 updated Resource Guide for Consumers: How to Access Mental Health and Substance Use Disorder Benefits.
2023 Resource Guide: How to Access Mental Health and Substance Use Disorder Benefits

February 2023
NH DHHS and UNH IHPP jointly hosted a stakeholder webinar regarding the March 31, 2023 end of continuous coverage and the Medicaid transition (‘unwind’) in an effort to share the latest information and resources, as well as field questions from our community partners and beneficiaries.
December 2022
At long last, health care providers and suppliers seeking to use patient incentives for contingency management to support evidenced based treatment for substance use disorder patients have guidance on how to minimize risk of fraud and abuse. Advisory Opinion, Office of Inspector General (OIG), posted March 2, 2022. Read about the risks, compliance tips and details.
March 2022
At long last, health care providers and suppliers seeking to use patient incentives for contingency management to support evidenced based treatment for substance use disorder patients have guidance on how to minimize risk of fraud and abuse. Advisory Opinion, Office of Inspector General (OIG), posted March 2, 2022. Read about the risks, compliance tips and details.
Legal Update on Fraud and Abuse Opinion on Contingency Management Program UNH Law

January 2021
Description: The paper highlights the need for New Hampshire to determine where it should invest broadband resources to close the digital divide that exists in the State between those who have internet access and those who do not; and equally as important, what modality of broadband infrastructure should be invested in to ensure equitable access to telehealth across New Hampshire and optimize broadband in the Granite State for the next 20-30 years.
2021
Advance Child Tax Credits start July 2021 as part of the federal COVID-19 relief package. Find out what you need to know.
May 2020
As part of the Medicaid expansion adopted in New Hampshire, the New Hampshire Department of Health and Human Services received waiver approval from the Centers for Medicaid and Medicare Services to implement Work and Community Engagement Requirements (WACER). This project explores the impact of the implementation of WACER on operations and infrastructure of community organizations. As well as exploring the expectations of "effort" by providers and community organizations to engage beneficiaries in the requirements.
June 2019
American Society of Law, Medicine, & Ethics in this report details changes in Medicaid Expansion in NH, the Granite Advantage Program, and the procedural history of implementation of Medicaid Expansion and the Work and Community Engagement Requirement (WACER)
American Society of Law, Medicine & Ethics (ASLME) 2019 NH Medicaid Work Requirement
April 2019
In this program Granite Advantage rules updates are discussed along with updates on key outreach and planned outreach activities. Following is provider, member, and stakeholder feedback, ending with online resources and a discussion on the digital outreach campaign.
February 2024
Develop a synthesis of tools and recommendations for collecting data from patients and clinicians related to primary care services and care delivery. Create a report of recommended tools that have been used and validated, ideally with an appendix of the actual survey instruments when they are available and can be used either with permission or for a fee.

Covering the Care: Health Insurance Coverage in New Hampshire
Individuals risk experiencing unexpected and high medical costs and often forgo necessary care when they lack health insurance. According to research by the Kaiser Family Foundation, 20% of uninsured people went without care, and another 24% postponed care, due to cost in 2015.
Covering the Care: Health Insurance Coverage in New Hampshire

Covering the Care: A Focus on the NH Marketplace
This brief provides background about what the New Hampshire Health Insurance Marketplace is, how NH residents are receiving coverage made available through NH’s federally-facilitated Marketplace in 2017, and how coverage is being accessed by the New Hampshire Health Protection Program.

Covering the Care: Cost Sharing Reductions in NH
This brief illustrates the extent to which individuals enrolled in Qualified Health Plans (QHPs) on NH’s Health Insurance Marketplace received Cost Sharing Reductions (CSRs), based on the most recent available detailed data (period November 1, 2015 – February 1, 2016).i More about the Marketplace in New Hampshire can be found in the policy brief, “Covering the Care: A Focus on the NH Marketplace,” published in June 2017.

Covering the Care: Medicaid, Work, and Community Engagement
June 2018
Over the next twelve months, New Hampshire will transition to a new coverage model for the Medicaid expansion program (the “Granite Advantage Program”), and will implement a demonstration waiver including a work and community engagement requirement, approved for New Hampshire on May 7, 2018.1 This brief focuses on the population covered by the New Hampshire Medicaid program, with an emphasis on work status and income (for a description of Medicaid expansion in New Hampshire, see Covering the Care: A Focus on the NH Marketplace).

Covering the Care: Health Insurance Coverage in New Hampshire | 2019 Update
December 2019
This brief provides updates from the Insurance Coverage and Marketplace “Covering the Care Briefs” that were previously published.
Covering the Care: Health Insurance Coverage in New Hampshire | 2019 Update

Covering the Care: Health Insurance Coverage in New Hampshire | 2020 Update
December 2020
This brief provides updates from the Insurance Coverage and Marketplace “Covering the Care Briefs” that were previously published.
This update also includes a special section focused on premiums and deductibles in New Hampshire.
Covering the Care: Health Insurance Coverage in New Hampshire | 2020 Update

Covering the Care: Legal Update December 2020
December 2020
Courts are deciding cases impacting how we access health care and insurance in New Hampshire. This Legal Update summarizes key health care cases including challenges to the Affordable Care Act, Medicaid work and community engagement requirements, due process rights for people with acute mental illness, state authority to regulate pharmacy benefit managers, and access to reproductive health.
Covering the Care: Legal Update December 2020

Covering the Care: Health Insurance Coverage in New Hampshire | 2021 Update
August 2022
This brief provides updates from the Insurance Coverage and Marketplace “Covering the Care Briefs” that were previously published by IHPP, providing information about coverage in 2020 and 2021. Please see “NOTE” in data sources to explain date changes and what is included.
Covering the Care: Health Insurance Coverage in New Hampshire | 2021 Update

Covering the Care: Health Insurance Coverage in New Hampshire | 2023 Update
March 2024
This brief provides updates from the Insurance Coverage and Marketplace “Covering the Care Briefs”
that were previously published.
Covering the Care: Health Insurance Coverage in New Hampshire | 2023 Update

Covering the Care: Hospital Consolidations Lead to Higher Healthcare Costs
2025
Time and time again, polls indicate that Americans are concerned about the cost of healthcare. It is one of the most prominent issues facing Americans1 because of affordability, access, and potential for debt.2 A July 2025 poll from Kaiser Family Foundation indicates that approximately half of U.S. adults say it is difficult to afford healthcare costs and about one third of adults say they have postponed care in the last year because of the cost.3 These concerns are not limited to those in the uninsured population; six in ten adults are worried about affording out-of-pocket costs not covered by insurance, such as co-pays and deductibles.4
Covering the Care: Hospital Consolidations Lead to Higher Healthcare Costs
The Association Between Childlessness and Loneliness in Later Life: Does Friendship Play a Moderating Role?
September 2025

Collecting, Sharing, and Using Information for Person-Centered Dementia Care: Perspectives of Residents, Care Partners, and Staff in Low-Resource Long-Term Care Settings
August 2025
Intersecting identities, inflammation, and sexuality: Effects of race, ethnicity, and education
September 2022
Intersecting identities, inflammation, and sexuality: Effects of race, ethnicity, and education

COVID-19 Factors Associated With Medication Changes Among Nursing Home Residents With Dementia
April 2025
COVID-19 Factors Associated With Medication Changes Among Nursing Home Residents With Dementia
Knowledge and Attitudes toward New Disease-Modifying Treatments for Alzheimer's Disease among Nursing Home Directors
January 2025

Changing attitudes about LGBTQ+ older adults: The Gen Silent Survey Project
March 2024
Lesbian, gay, bisexual, transgender, queer, and more (LGBTQ+) older adults may experience challenges accessing services due to stigma. Aging service providers seeking to create an inclusive culture need training tools. This study examined if a film (Gen Silent) could increase provider’s knowledge of and empathy for LGBTQ+ older adults.
Changing attitudes about LGBTQ+ older adults: The Gen Silent Survey Project
Geographic Variation of Antidementia and Antipsychotic Medication Use Among US Nursing Home Residents With Dementia
August 2024
Several antidementia medications have been approved for symptomatic treatment of cognitive and functional impairment due to Alzheimer disease. Antipsychotics are often prescribed off-label for behavioral symptoms.

April 2019
UNH College of Health and Human Services held a half-day summit of learning, networking, and exploration regarding long term care research. Sessions focused on current trends in research and the practical application of solutions from both a direct care and systems-based perspective.
November 2018
While everyone’s natural process of aging is different, most individuals will need some form of assistance as they age. This might include medical attention, help with meals, or receiving assistance with daily activities – and often includes several different services, simultaneously. Trying to keep up with medical and social needs requires coordination and communication among systems of care. In the absence of integrated coordination, people can have inefficient, frustrating, and even unsafe experiences. Given this landscape, systematic support as people age is critically important.
Developing a Foundation for Integrated Care Coordination: Part 1
June 2018
NH health insurance coverage data showcase as of June 2018.
July 2016
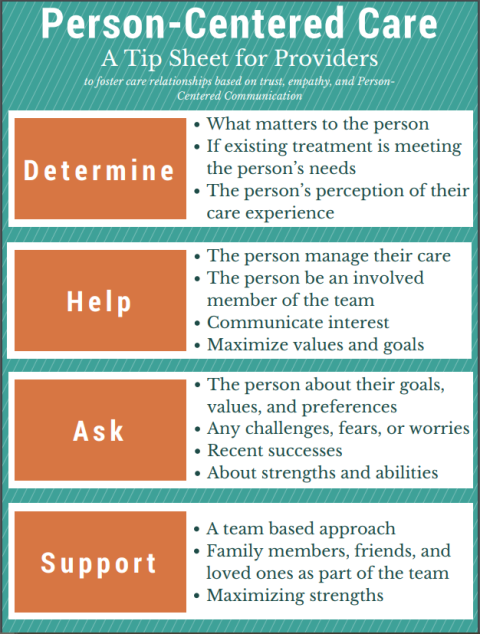
The physician-patient relationship has always been centered around the physician, with the Center on Aging and Community Living's "Person-Centered Care" video the relationship is reversed. Learn more about the benefits of the physician-patient relationship getting reversed.

July 2017
The following video was created as part of a training for the Practice Transformation Network. The training focuses on person-centered care transitions in a medical neighborhood.

December 2015
Citizens in the U.S. are making organized efforts to demand a new approach to planning urban communities, one that results in more sustainable and livable communities. The profession of social work in the U.S. once had a primary role in organizing urban residents to advocate for healthier environments in their neighborhoods. Yet, recent research documents the diminishing emphasis on community organization as an intervention method in social work. This paper offers a descriptive case study of a successful community organizing effort to promote a more livable city in Portland, Maine (USA).
A Case Study in Organizing for Livable and Sustainable Communities
Winter 2015
This paper examines the lack of advocacy for senior issues in the Granite State and explores strategies that can be employed to grow grass-roots leadership among older adults. The New Hampshire Senior Leadership Series, a program that provides support and training in advocacy and leadership skills, is highlighted as a promising practice to address this need.
September 2015
In a collective impact approach, the work begins with a shared understanding of the key challenges and opportunities before us and a commitment to solving it together through agreed upon actions and strategies. The process starts with mapping the landscape. This significant work by the Center on Aging and Community Living (CACL) at the University of New Hampshire is a knowledge base from which we will create shared goals, identify existing and emerging strategies and set a course for creating the elder-friendly communities we all want to live in as we age.
Environmental Scan to Help Create Elder-Friendly Communities in NH
Winter 2014
In the fall of 2012, the Center on Aging and Community Living (CACL) at UNH, with funding from the New Hampshire Endowment for Health, convened a series of meetings with key stakeholders to consider the future of New Hampshire’s system of Long Term Services and Supports. This paper summarizes that work. In response to mounting concerns about the impact of an aging population on our state, the New Hampshire Center for Public Policy Studies (NHCPPS) produced two reports - New Hampshire’s Silver Tsunami: Aging and the Health Care System; and Aging and the Public Long Term Care System. These reports frame the issues that New Hampshire is facing as it confronts the challenge of meeting the needs of an increasingly older population.
Winter 2014
In the fall of 2012, the Center on Aging and Community Living (CACL) at UNH, with funding from the New Hampshire Endowment for Health, convened a series of meetings with key stakeholders to consider the future of New Hampshire’s system of Long Term Services and Supports. This paper summarizes that work. In response to mounting concerns about the impact of an aging population on our state, the New Hampshire Center for Public Policy Studies (NHCPPS) produced two reports - New Hampshire’s Silver Tsunami: Aging and the Health Care System; and Aging and the Public Long Term Care System. These reports frame the issues that New Hampshire is facing as it confronts the challenge of meeting the needs of an increasingly older population.

2014
The ten chapters of this manual include easy to follow, pragmatic steps to implement a comprehensive approach to hypertension care originally developed by CMC/DHK. This approach was successful in improving hypertension control for the greater Keene community, and was successfully replicated in the communities of Manchester and Nashua. The first seven steps are best implemented sequentially, whereas steps eight through ten can be undertaken anytime, as they involve patient and community engagement. However, considering that each medical practice and community is unique, the steps can be customized to accommodate the distinct degree of readiness or available resources.
IHPP Training and Resources
With funding available through the Maternal Opioid Misuse Model (MOM), a team from IHPP collaborated with the Perinatal Substance Exposure Collaborative, to develop a comprehensive resource guide to support perinatal and postpartum individuals in New Hampshire.
Supporting the Perinatal and Postpartum Population: A Community Resource Guide for NH includes 74 pages of resources ranging from prenatal healthcare to substance use treatment, community mental health centers, parenting supports, supports for children, housing assistance, legal assistance, apply for state assistance, transportation, and interpersonal violence crisis resources. Edits and additions can be submitted by emailing ihpp.unh@unh.edu.
Prove It! Let the Data Tell the Story is a hands-on course focusing on the use of data and basic statistics commonly used in public health. NH community leaders expressed the need for training about using data to support their efforts to improve the health of their communities, and Prove It! was conceptualized by the Empowering Communities project to meet that need. Prove It! provides a basic understanding of why we use data and how to use data in community health assessment and monitoring, using the specific focus on writing grant applications as the example.
For more information on having Prove It! taught in your organization, send an email to IHPP.UNH@unh.edu.
IHPP Grand Round Series
During this session, members of IHPP shared a selection of our work related to Mental Health and Substance Use Disorder (SUD) policy and treatment.
Watch the recording from March 31, 2022 below: